Mobile Menu
- Education
- Research
-
Students
- High School Outreach
- Undergraduate & Beyond: Community of Support
- Current Students
- Faculty & Staff
- Alumni
- News & Events
- Giving
- About
Katie Sullivan

Researchers at the University of Toronto and University Health Network have found that standard pathology grading for the most common type of pancreatic cancer can be improved to better predict patient outcomes.
The research shows that conventional, histological analysis of pancreatic tumours — based in part on morphology, or shape and structure — can better predict outcomes by taking into account particular tissue patterns that correlate to molecular analyses, shown to be more precise.
The researchers were able to stratify the tumours into two groups. Those that showed 40 per cent or more aberrant, destructive patterns, such as cells with punched out spaces resembling swiss cheese, matched the molecular profiles of tumours from patients with poorer survival.
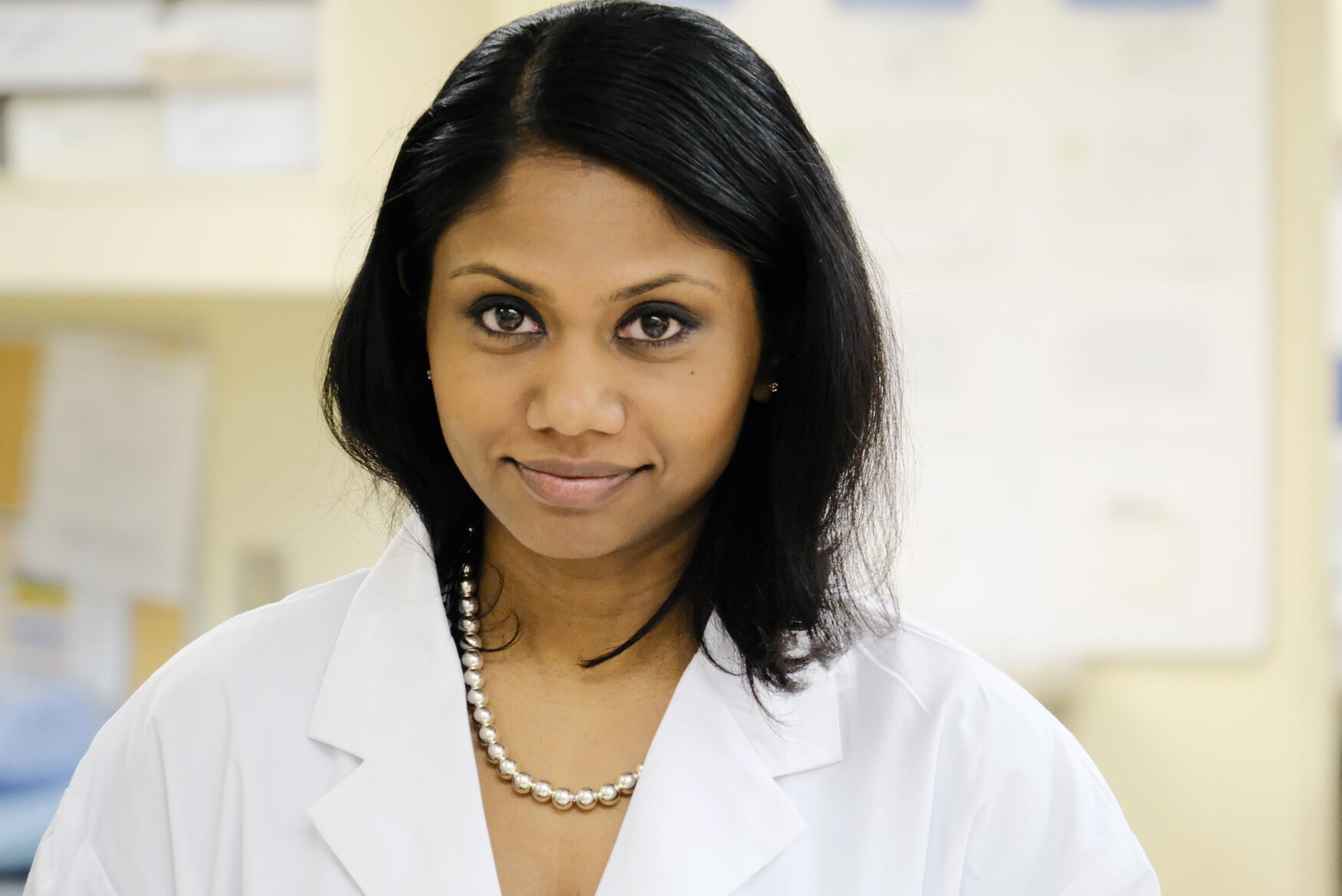
“Although we have been aware of these patterns, putting them together with an established threshold indicating levels of aggressive tumour patterns is new and helpful for our clinicians,” says lead author Sangeetha Kalimuthu, a professor of laboratory medicine & pathobiology at U of T and a gastrointestinal pathologist at UHN.
The study involved over 800 tumour tissue slides from 86 patients with pancreatic ductal adenocarcinoma. The study group included senior author Runjan Chetty, also a professor of laboratory medicine & pathobiology at U of T and a clinician-scientist at UHN, and colleagues at Princess Margaret Cancer Centre and the Ontario Institute for Cancer Research.
The journal Gut BMJ published the findings online last week.
For decades, histological evaluation has been the gold standard for diagnosis of pancreatic cancer. Recently, large-scale studies have shown that molecular subtypes of the cancer are associated with various prognoses.
But molecular profiling is expensive and requires specialized equipment. With the new, easily applicable pathology classification, Kalimuthu and her colleagues believe that clinicians can obtain similar information using standard pathology stains, with a rapid turn-around time.
“Any pathologist in any part of the world can do this,” says Kalimuthu. “It’s the bread and butter of what pathologists do. It’s fast, cheap and accessible.” The new classification should help clinicians better tailor treatments to patients, she adds.
Pancreatic ductal adenocarcinoma is one of the most lethal cancers, with a five-year survival rate of less than 10 per cent. Each year more than 350,000 people worldwide are diagnosed and more than 340,000 die of the disease. Some reports project a twofold increase in the number of new cases and deaths by 2030.
“Pathologists have had a long, rich history in their vital roles to diagnose and stage pancreas cancer,” says Steven Gallinger, a co-author on the study who is a professor of laboratory medicine & pathobiology at U of T and a clinician-scientist at UHN. “This study is an elegant demonstration of the potential of personalized medicine, with the promise of improved outcomes for our patients.”
The next step for the researchers is to carry out a multi-institutional validation study. They also hope to develop artificial intelligence, deep-learning algorithms to further reduce turn-around times and increase accuracy. The longer-term goal is to help pathologists accurately quantify even large amounts of data.