Main Second Level Navigation
Breadcrumbs
- Home
- News & Events
- Recent News
- Respirologist Dr. Chung-Wai Chow: Advancing Understanding of Lung Health
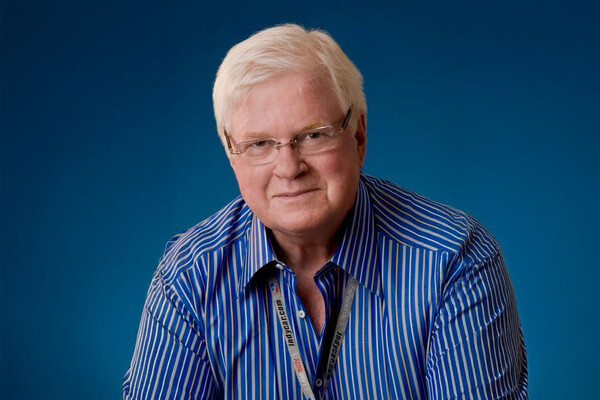
Respirologist Dr. Chung-Wai Chow: Advancing Understanding of Lung Health
Dr. Chung-Wai Chow is the first graduate (in 1999) of the Department of Medicine’s Eliot Philipson Clinician-Scientist Training Program, a competitive program that enables medical residents to pursue graduate-level research training. She works as a physician in the University Health Network’s Lung Transplant Program, the largest such centre in the world. In her clinical work at UHN, and through her research at the Toronto General Research Institute, Dr. Chow studies how environmental air pollution affects cardiorespiratory health. She is also an associate professor at U of T’s Faculty of Medicine with cross-appointments to the Dalla Lana School of Public Health and Faculty of Applied Sciences and Engineering. She is also a faculty member with the Faculty of Medicine’s Institute of Medical Science and the President of the Humboldt Association of Canada.
The biggest thing I learned was to think like a scientist. The Eliot Philipson Clinician-Scientist Training Program recognizes that dedicated research training is critically important for clinicians who wish to pursue research.
The very first graduate of the Department of Medicine’s Eliot Philipson Clinician-Scientist Training Program, Dr. Chung-Wai Chow, explores how environmental air pollution affects cardiorespiratory health. We asked about her innovative approaches to studying respiratory illness, her recent findings and her advocacy to enhance lung disease intervention in Ontario.
You are leading a five-year study funded by the Canadian Institutes of Health Research on the link between air pollution and lung transplantation. How will it help shed light on chronic airway inflammation?
Indoor and outdoor air pollution is responsible for millions of deaths annually related to respiratory illness. In Canada, we often don’t think this issue applies here, and we enjoy one of best air qualities in the world, but there’s still a lot we don’t know about the underlying biological mechanisms of lung disease. With post lung-transplant patients, whose health we track over time, we have an almost perfect model to better understand the long-term effects of air pollution, and we’ll get better answers than if we study a population of random people in Toronto. The insights are highly applicable to patients with other chronic airway diseases, such as asthma and chronic obstructive pulmonary disease.
This research involves collecting data from pollution-tracking devices that participating transplant patients wear and place in their homes for certain periods of time. What key insights have emerged so far?
We are getting a better understanding of how a person’s exposure is affected by the ambient air pollutants in their community. We’re also learning about the contributing role of home environment factors such as location upwind or downwind from a highway, the building materials used for construction, the types of cooking fuels they use, if there is an attached garage with a doorway to the home, and if a fireplace is used. We are now analyzing how the results compare to existing research showing that patients who live in high-traffic, dense urban areas are at increased risk of developing chronic lung rejection. We are seeing a clear connection between exposure to traffic-related pollutants, indoor air pollution and lung function.
You are also conducting two other studies on how air pollutants affect lung health in specific geographic areas — why is it important to understand these regional differences?
The chemical compositions of air pollutants in Toronto are very different from those in London, Paris or Fort McMurray. I collaborate with U of T engineering professors, as well as scientists from Environment Canada, to create a novel simulation system for mice models that mimics typical exposure situations of humans in different regions of the world by replicating specific combinations and concentrations of pollutants. It lets us study the impact of exposure to different types of pollutants, such as from vehicle exhaust or industrial facilities. This type of repeated-exposure system is one of only two in North America. The better we understand the specific nature of pollution-caused airway inflammation, the better we can develop more targeted and effective medical interventions.
You have cooperated with the Ontario Lung Association to advocate for political action to improve lung health in Ontario. What kind of strides have you made, and what still needs to be done?
After 10 years of lobbying, we were able to get the Lung Health Act passed in 2017 — it recognizes that lung diseases present a significant health burden in terms of use of health care resources and loss of economic productivity. And it increases the government’s focus on addressing this problem. The biggest challenge now is to better fund research into lung disease, which falls so far below the funding rates for other, even rarer, diseases. Also, I’d like to see better planning of public spaces so that we don’t put schools, playgrounds or seniors’ homes next to a road, and plant more trees to filter out pollutants.
As the first graduate of the Department of Medicine’s Clinician Scientist Training Program, what was your biggest takeaway from the program? In what way did the University of Toronto help shape your career?
The biggest thing I learned was to think like a scientist. The thought processes involved in framing research questions and ways to address them are fundamentally different from clinical practice. While clinicians have specific insights derived from our practice that allow us to ask questions that are not apparent to non-clinicians, the Eliot Philipson Clinician-Scientist Training Program recognizes that dedicated research training is critically important for clinicians who wish to pursue research.
I am also particularly thankful to have had great mentors at U of T. Dr. Charlie Chan taught and continues to teach me the meaning of integrity in all its forms. Professors Eliot Phillipson and Arthur Slutsky are simply incredible clinician scientists who have made seminal discoveries over their careers. Despite their busy schedules, they were able to make time to meet with me regularly when I was a trainee. Prof. Slutsky, in fact, made a point of scheduling regular lunch meetings with me to make sure my training was on track. I respect them hugely. They have and continue to provide me with guidance and support as my career progresses.
What advice would you have for current students and trainees?
Like what you do — in and outside of work. Like the people you work with, as you will be spending a lot of time with them over the course your life. Get the best training possible. Go abroad for training. And very importantly, keep your eye on the ball: what are the current biomedical issues, in what direction is the field heading? Because at the end of the day, you need funding to conduct research, so you will need to follow the research dollars.
— in conversation with writer Sharon Aschaiek, photo by Sepehr Salehi
News