Mobile Menu
- Education
- Research
-
Students
- High School Outreach
- Undergraduate & Beyond: Community of Support
- Current Students
- Faculty & Staff
- Alumni
- News & Events
- Giving
- About
It’s been more than a year since the start of the COVID-19 pandemic. In that time, there’s been an exponential growth in demand for microbiology services.
After the pandemic started and needs for COVID-19 test processing skyrocketed, microbiology labs suddenly had to adapt to a new environment and grow rapidly, as resources in hospitals shifted to address the pandemic.
Microbiology spans both clinical and laboratory services.
Experts in microbiology bring knowledge in infectious diseases, testing modalities, laboratory operations, quality control and diagnostics.
They’re a vital part of the fight against COVID-19.
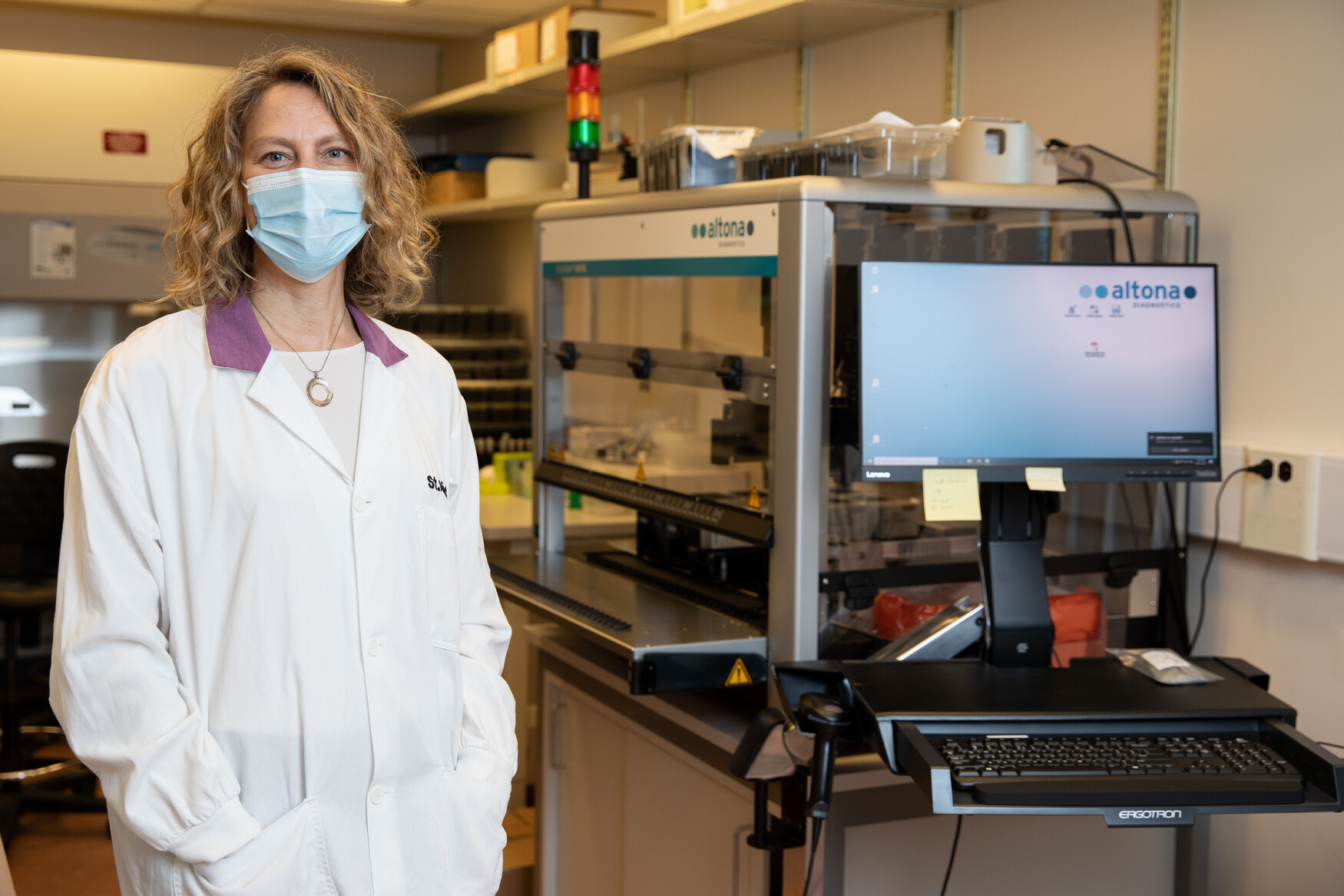
“In early 2020, we started our own in-house testing for COVID, processing around 20 patient specimens a day. Now, we routinely test around 1,500 specimens a day,” explains Larissa Matukas, an associate professor in the Department of Laboratory Medicine & Pathobiology at the Temerty Faculty of Medicine and Head of Microbiology at St. Michael's Hospital of Unity Health Toronto.
After COVID-19 hit, a dedicated team worked around the clock at St. Michael’s to scale up laboratory services, including procuring equipment and reagents, and bringing in more staff and conducting training.
“Everyone recognized the need we had, not just on a hospital level, but on a community and public health level. COVID-19 meant all hands needed to be on deck,” says Matukas.
The laboratory at St. Michael’s has grown as large as the space will allow, already taking over office spaces to accommodate necessary equipment. It is still undergoing renovations.
The lab has been able to meet the demand of their acute care facilities across Unity Health, which includes St. Michael’s Hospital, St. Joseph’s Health Centre, Providence Healthcare, in addition to other long term care homes and other community locations.
Procurement and supply-chain management has now become almost a full-time occupation, says Matukas.
“There were global supply chain issues at the start of the pandemic. Those issues are still very much in play, not just for COVID testing, but for all other aspects of microbiology testing and other areas of laboratory medicine and research. A lot of the instrumentation and supplies that we use are very hard to come by,” she says.
Scaling up personnel has involved teamwork across multiple disciplines, says Matukas.
Many people had to be trained in the necessary techniques for PCR (polymerase chain reaction) testing.
“A lot of medical lab technologists have not been trained to do that type of work before, so we've trained them from the ground up,” explains Matukas.
“Some have come with experience, but very few had been trained on the equipment that we have. We had to learn so much ourselves.”
Matukas and her colleagues trained redeployed personnel from various research areas, and other lab disciplines to scale up and support all steps in the COVID testing process.
Anatomical Pathologists were trained to work alongside the growing team of core medical microbiologists to oversee quality assurance, result verification and report sign out to meet the expansion demands.
The team at St. Michael’s has also played a role in thinking differently about testing in the pandemic.
“We've been looking at different kinds of specimen collection devices, at how we can detect COVID in other types of specimens that are collected from patients. We’re thinking about how we can use whole genome sequencing to identify the different strains that are circulating, and how to optimize operations and workflow processes,” adds Matukas.
“It's been a whirlwind year.”
Despite being in a peak of infection rates, Matukas says hospital admissions and testing plans still need to be determined for the future.
For example, what will the scope of testing and practice be after the pandemic?
If COVID does not go away, as Matukas predicts, how will services respond to that?
Matukas is also concerned about the pressure the healthcare system has been under for months.
“What we are going to witness is the effects of having a whole system that is burnt out. How are we going to recover? How can we make sure we can all keep going and come out stronger?,” she says.
Most importantly, Matukas wants to figure out the best way to proceed, and lessons from the pandemic.
“My hope is that we actually do take something away that is maintained and sustained. Although it’s been amazing to witness how hospitals and laboratory personnel across multiple disciplines have come together, we need to make sure hospitals are sufficiently supported to handle the next public health infectious disease crisis,” she says.

