Main Second Level Navigation
Breadcrumbs
- Home
- News & Events
- Recent News
- MD Photo Sharing App Creator: Dr. Joshua Landy, PGME ’11
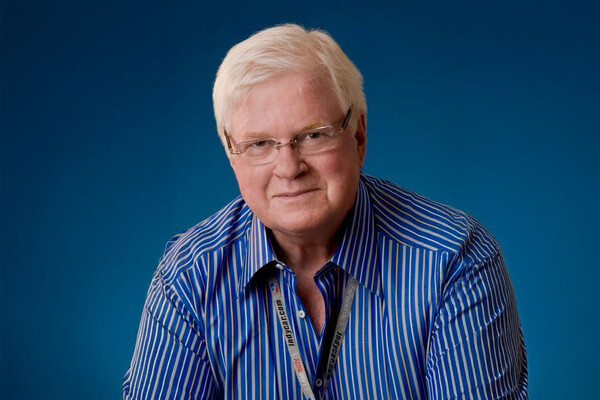
MD Photo Sharing App Creator: Dr. Joshua Landy, PGME ’11

Dr. Joshua Landy, PGME ’11 (Critical Care) is a critical care specialist, having completed his M.D. at the University of Western Ontario, his internal medicine residency at the University of Alberta, and his critical care fellowship at the University of Toronto.
In 2013, Dr. Landy co-founded a venture capital funded mobile health startup called Figure 1, a free-access medical case-sharing platform with more than 1.5 million users from all over the world, 2 million views a day and accessed by 70% of medical students in North America.
I don’t think the knowledge of medical specialists should be beyond reach of anybody with an internet connection.
What inspired you to start Figure 1, the medical image repository and smartphone app?
After working at a number of hospitals in the GTA, I noticed mobile phones were being used to communicate about patients. Physicians and students were taking pictures and then texting or calling colleagues with questions — it was an efficient and valuable practice, and it made me curious about what greater trends it indicated.
I later went to Stanford to study how young physicians were using their smartphones and found the same behavior as I had observed here. While physicians were doing this for many different reasons — some to ask for help, some to teach, and some to document an unusual or extreme example of a case — I realized there was tremendous opportunity in all of that data. The conversations amounted to incredibly concentrated assets of medical education, but were being lost in the bottom of people’s inboxes. They were not being indexed or archived in any meaningful way, and there was no privacy protection either. That was the catalyst which inspired Figure 1, a platform where people could put their images and hold those conversations and have it all viewable and findable for people to learn.
You now have more than 1.5 million users from around the world, 2 million views a day and around 70 per cent of medical students in North America are using Figure 1. How does it work?
We have been using smart phones in our lives for the last decade or so, and the camera has been an important part of that experience. We use photographs and short conversations to relay so much meaningful content that it is entirely applicable to health care, which needs an efficient way of communicating.
So with Figure 1, we’ve created a smartphone-based system that replicates processes that physicians are familiar with, for example, our Paging feature. This behavior is analogous to how a physician might call the hospital switch board and ask for a specialist who would then be paged. With Figure 1 you can get an answer from a verified specialist within an hour which is way faster than any hospital I’ve ever worked in. Many students who are looking to learn about a particular topic also find the platform valuable.
What is the most unexpected result you’ve achieved so far through Figure 1?
I was surprised at how rapidly it was adopted. We expected a slow start and we had a staged roll-out first in North America then England and the rest of the English speaking world. Instead, it was adopted on a global scale surprisingly quickly, so after that we essentially rolled out whenever the legal work was completed. We worked with over 40 different law firms around the world to create a tool that is safe, secure and takes into account privacy concerns in 190 countries around the world. Aside from North America, we were surprised at the uptake in Brazil, so that necessitated translating the app to Portuguese and then to Spanish to serve users in Latin America. Our consent form, which is built in for physicians to show their patients, is now available in over 60 languages.
You did your critical care fellowship at the University of Toronto. What kind of opportunities did U of T offer you?
Toronto has become an epicenter for innovative research in critical care, so I knew I would have the opportunity to work with a number of brilliant and high-profile opinion leaders in the field of critical care — and the best teachers and researchers in the world. My training gave me a robust appreciation of the current state of the medical literature as well as the ability to critique it and understand it. Some of my colleagues don’t necessarily possess the ability to deconstruct or critique a piece of literature the way I learned to do and it’s provided me with a more incisive view of medical data.
Critical care training at U of T is unique because you don’t just stay in one hospital, but rotate through sites and get a broad view of critical care. The variety was something I don’t believe you can get anywhere else. It gives you exposure to differences between very smart physicians, which can be very nuanced, whether it is when to start a certain medication or triaging patients differently. When you have a wide variety of experience you can choose to take what you find valuable and leave behind what you don’t. This is also one of the core values of Figure 1 — to create a process that is uniquely your own and uniquely suitable to you.
What are the next big challenges you’ll be taking on?
The challenge for us at Figure 1 is to democratize the knowledge of medicine. I don’t think the knowledge of medical specialists should be beyond reach of anybody with an internet connection. Whatever we do next will be in service of that goal. Being able to give good medical care, and to get the information you need in the moment you need it, is something that we can achieve today. We can give ourselves the best health care system in the world by bringing knowledge together and making it accessible.
News