Main Second Level Navigation
Mar 2, 2022
The Future of Organ Transplantation
Research, Education, Faculty & Staff, Partnerships

UHN
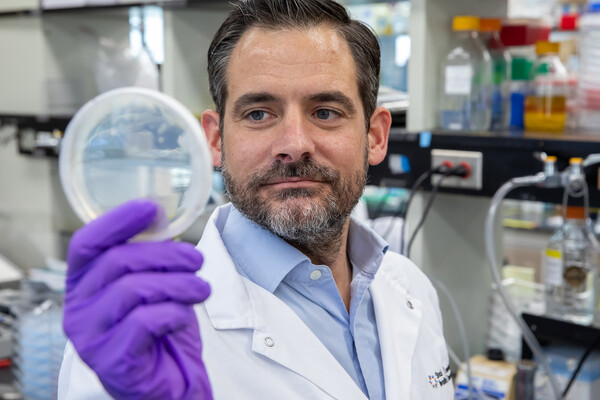
At Prof. Marcelo Cypel’s laboratory, Aizhou Wang (pictured) demonstrates how the cocktail of enzymes that were used in this study are delivered to a donor lung using the Ex Vivo Lung Perfusion system.