Mobile Menu
- Education
- Research
-
Students
- High School Outreach
- Undergraduate & Beyond: Community of Support
- Current Students
- Faculty & Staff
- Alumni
- News & Events
- Giving
- About

Gabrielle Giroday
A company founded by two University of Toronto researchers will be manufacturing a portable ventilator that will help Canadian patients with COVID-19.
The portable intensive care unit can be operated by battery power. It has a ventilator and can do vital signs monitoring, among other features.
The device was originally developed to treat members of the military who had been critically injured in operations and needed to be transported.
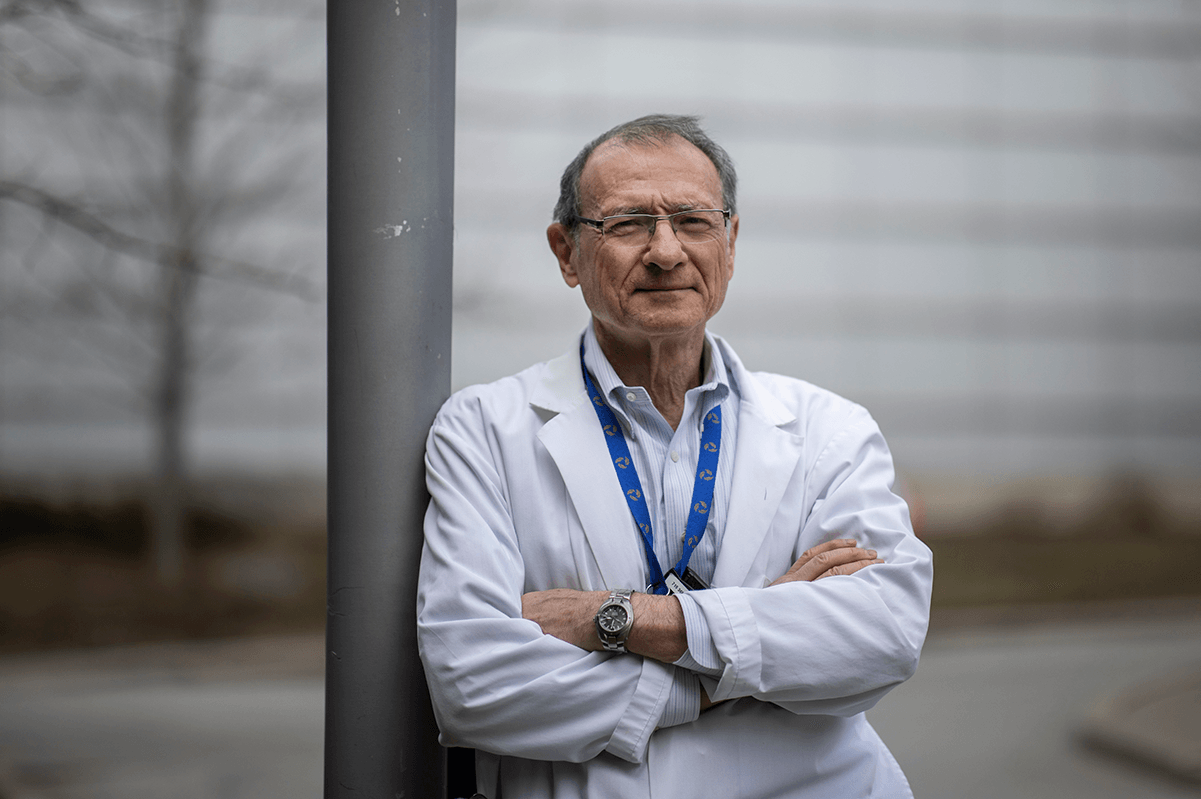
The technology will now be manufactured to assist patients who need life support due to the current global pandemic, says Dr. Joe Fisher, a professor in the department of Anesthesiology and Pain Medicine at University of Toronto’s Faculty of Medicine and staff anesthesiologist at Toronto General Hospital in the University Health Network.
“I think that this device has several roles in the COVID-19 pandemic. The first role is to help with a surge in supply — if you want to open up a new ICU bed, all you need is this and a stretcher, and you can do that,” says Fisher, who is co-founder of Thornhill Medical, which sells the device.
The company was cited by Prime Minister Justin Trudeau in a speech Friday morning focusing on Canadian innovators who will be helping in the fight against COVID-19.
“Dr. Fisher and his colleagues have always thought ahead, ‘What if? What if these devices were needed to support large numbers of patients?,’” says Dr. Beverley Orser, professor and chair of the department of Anesthesiology and Pain Management.
“They have used their creativity, knowledge and ability to form teams to create these technologies, so we can share them with the world. Dr. Fisher has always been committed to doing the right thing, and sharing technology to support others. He is an incredible innovator.”
Thornhill Medical was founded in 2004 by Fisher and Dr. Ludwik Fedorko, an associate professor in the department of Anesthesiology and Pain Medicine, as a spin-off of the University Health Network and University of Toronto.
Fisher says his hope is that the device will provide life support and vital signs monitoring to those in dire circumstances, if needed.
“I think that its main function is to provide a compact platform to provide critical care. It may also provide back-up care when there is no electricity and when no oxygen is available,” says Fisher.
There are also other important features, he says.
“This was also designed with transport of patients in mind, such as if you need intra-hospital transport, to take a patient from the ICU bed to CT scan or to the operating room. Right now, it’s extremely challenging to do that,” says Fisher, explaining that it takes a significant amount of effort by staff to move a patient.
“This device is easily attached to a hospital bed or stretcher, provides all the ICU functions to the patient, and you just roll out the bed, and can move them. If the patient needs to be transported to another hospital, it simply fits into the ambulance at the patient’s side continuing the same level of life support.”
There have been widespread concerns expressed about the availability of ventilators for COVID-19 patients as the number of people who have contracted the disease has shot up.
While the portable intensive care unit will now be used as part of the response to COVID-19, the inspiration for the device dates back more than 15 years.
“I came to the attention of the United States Marine Corps around 2004, when they were looking for a device that would get rid of their use of oxygen tanks in the field,” says Fisher.
The move away from using oxygen tanks in portable intensive care units during overseas military operations was because the oxygen tanks were targeted as explosive devices in battle, he adds.
"We were the first to provide the Marines with the capability of providing injured patients with high oxygen concentrations without use of oxygen tanks. Once created, the device was tested the Marines engaged us to add more and more features including the ability to ventilate patients. Then they wanted to extend the design so it can be used during transport in a helicopter or aircraft, or ground transport vehicle, while a person remained on life support," says Fisher. "These features had to be invented from scratch, and integrated with each other. And they were, even if it took five or six years."
Fisher says the portable intensive care unit was the result of a concerted effort by a group of people.
“First of all, it’s compact. Our device weighs about 40 pounds and works off batteries. In all other devices, batteries are for temporary use and need to be plugged in,” says Fisher. “It’s completely self-contained, what you have in that little box, is everything that there is in an intensive care unit, all the monitors, the ventilator, and the oxygen. But in this case the oxygen doesn’t come from a tank but from the air.”

