Main Second Level Navigation
Oct 11, 2023
Study uncovers how the gut's microbiome boosts immune system development
Students, Research, Education, Faculty & Staff

Mark Bennett
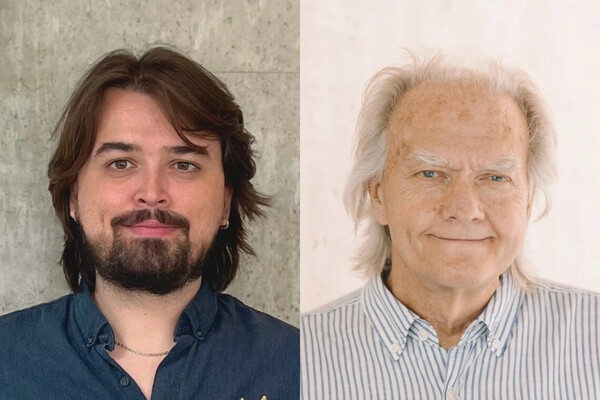
Arthur Mortha, left, and Pailin Chiaranunt led research that revealed new insights about how gut microbes influence immune system development