Mobile Menu
- Education
- Research
-
Students
- High School Outreach
- Undergraduate & Beyond: Community of Support
- Current Students
- Faculty & Staff
- Alumni
- News & Events
- Giving
- About

Ciara Parsons
To create more awareness and better prepare early-career physicians to care for LGBTQ+ patients, a team from the University of Toronto have developed a new LGBTQ+ health workshop for resident physicians.
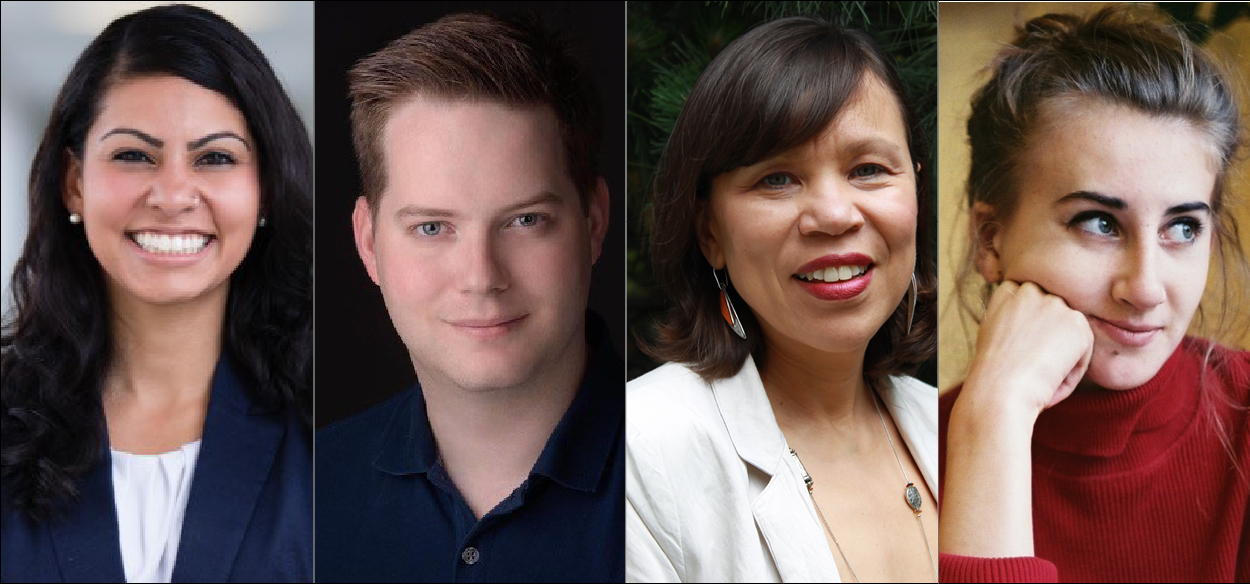
Drs. Tehmina Ahmad, Michael Scott and Jacqueline James, a professor with the Department of Medicine, alongside Wilson Center Researcher Miranda Schreiber, developed this workshop as a way of calling attention to the unique needs and health disparities faced by LGBTQ+ people.
“It is dangerous to look at LGBTQ+ issues and view them as being the same as anyone else’s. We need to be able to explore the complexities of LGBTQ+ issues,” said Ahmad, a fourth-year resident physician in the University of Toronto’s Department of Medicine.
“If we take on the mentality that everyone is the same, it really limits our ability to appreciate individualism and celebrate multiple gender identities. It’s an act of erasure and minimizes the struggles of LGBTQ+ folks.”
The lecture launched on June 24th and is geared towards second-year Internal Medicine. It includes a comprehensive overview of LGBTQ+ history, politics, race, systemic barriers to health and how these issues intersect and contribute to the ‘LGBTQ+ health gap’.
Ahmad says evidence of the LGBTQ+ health gap can be seen through the host of health conditions LGBTQ+ people are overrepresented in and how on average they live shorter, less healthy lives than cisgender, heterosexual people.
“We know that LGBTQ+ folks are less likely to have a family doctor and they’re more likely to develop chronic diseases. We also know LGBTQ+ folks are more likely to be affected by mental health and substance dependency disorders. These are all intersectional issues that contribute to the LGBTQ+ health gap,” said Ahmad.
Under-utilization of health care services – even those that are medically necessary – is a chronic issue within the LGBTQ+ community and has been exacerbated by negative interactions with health care providers and the health care system. Not feeling heard by health care providers or included in their own care are concerns often voiced by LGBTQ+ people, particularly those that are racialized, say the team members.
To combat this and help physicians to understand how they can make LGBTQ+ patients feel more welcome, the group’s lecture series includes information about safe care and inclusive spaces, say team members. Through mock scenarios and ‘tips for care’ slides, the group offers suggestions as to how physicians can approach LGBTQ+ patients.
“There is a huge power and privilege difference between health care providers and our LGBTQ+ patients—and we as physicians should be using it to intervene and advocate for our patients and be allies to them so we can create better outcomes for this population,” said Ahmad.
As a way of continuing this work and ensuring medical trainees and physicians possess a baseline understanding of LGBTQ+ health, the group is working on a project with the help of Dr. Saleem Razack of McGill University. They are developing a position paper that highlights LGBTQ+ health outcomes and hope it will lead to the establishment of a national LGBTQ+ curriculum standards.

