Mobile Menu
- Education
- Research
-
Students
- High School Outreach
- Undergraduate & Beyond: Community of Support
- Current Students
- Faculty & Staff
- Alumni
- News & Events
- Giving
- About
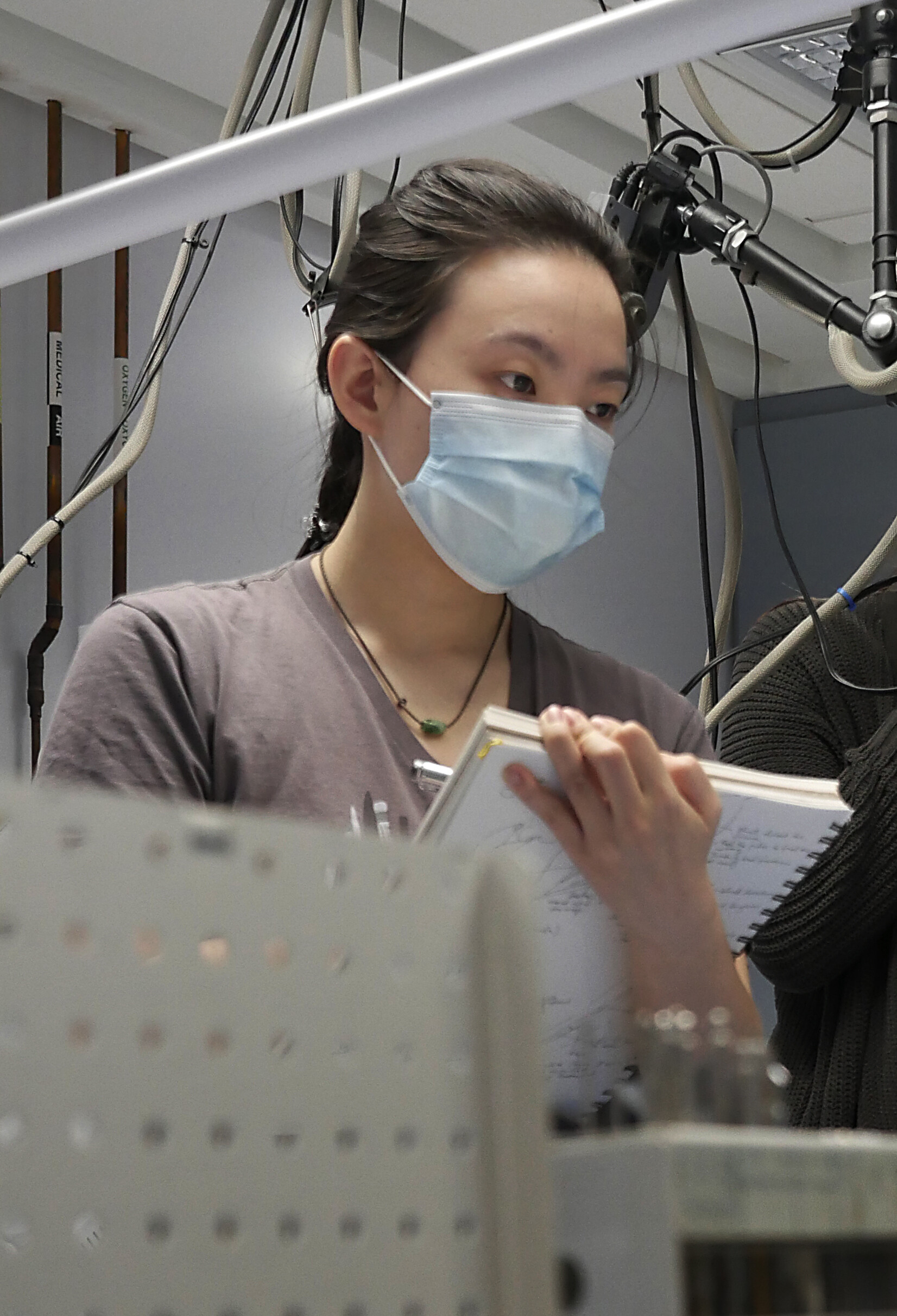
Every year, students in the Master of Science in Biomedical Communications go into a hospital operating room to get experience sketching surgical procedures.
However, in 2021, the COVID-19 pandemic meant restrictions on who could enter hospitals, and surgeries were limited to essential personnel only.
Shelley Wall, an associate professor in the Biomedical Communications (BMC) program, and Lisa Satterthwaite, senior manager of the University of Toronto’s Surgical Skills Centre at Mount Sinai Hospital, wanted students in the program to have the chance to watch a surgeon operate on a patient.
So, in May 2021, Wall and Satterthwaite decided to create a surgical observation session specifically for first-year graduate students in the program.
“After the third wave of COVID-19 hit, we knew students would not be able to enter the operating room. However, we needed to find a way for them to gain training,” said Wall.
The session happened on May 6.
Students attended a session in-person at the University of Toronto Surgical Skills Centre at Mount Sinai Hospital, while following strict COVID-19 protocols.
The centre is a laboratory setting where surgeons, medical students, residents, fellows and physicians can learn and practice basic and complex surgical and medical procedures.
"I contacted a few surgeons who spoke with their residents to see who would be interested in doing a surgical observation session. Five residents responded and volunteered to come in and perform surgical procedures on tissue," says Satterthwaite.
BMC students observed residents as they performed orthopaedic trauma surgery in the Surgical Skills Centre’s training theatre.
To prepare the students for surgical observation, Wall lectured them in advance on the basics of surgical procedure.
Wall instructed students on how to tell a story through a series of images – what’s known as “the visual narrative” by biomedical communicators.
During the session, students observed techniques such as plating of fractures and tissue dissections.
Aimy Meng Yu Wang, a biomedical communications graduate student, compared sketching the surgical demonstrations to figure drawing.
“We only had a short amount of time to capture a movement, a sequence, a set of steps – so every stroke had to count,” says Wang. “It was great that we were able to attend a surgical training session because we could ask the residents questions directly. This would have been much more difficult to do in the operating room.”
Surgical illustration skills are transferable to all aspects of medical illustration and animation, says Wall.
“Students have to bring to bear all the anatomical and procedural knowledge they are gaining. This experience crystallizes what needs to be done to tell a good visual story,” she says.
Since the May 6 session, Satterthwaite has been able to offer a second observation session for BMC students with the cardiac resident training program.
“We are grateful to the Department of Anatomy for their support. Without them, these sessions would not have been possible,” she says.

